If you’re reading these words, chances are you (or someone you love) are suffering from a lower quality of life because of ulcerative colitis, and you most likely got here from a Google search for Ulcerative Colitis Diets. (or you may have seen this posted on Facebook or another social channel but Google is much more likely)
You probably already know that chronic inflammation of the colon (either parts or the entire colon) is the hallmark symptom of ulcerative colitis. You already know that this inflammation often causes the tissue lining the colon to break down, forming ulcerations that can bleed and result in bloody diarrhea.
And you’ve likely heard that it’s almost always deemed necessary for ulcerative colitis to receive “treatment” and are actively looking for alternative or less invasive options. Of course, as with all dis-ease, DIET is an excellent place to start the healing.
Unlike most articles like this that you’ll find online, I’m going to get right to the point. However, if you want to learn more about ulcerative colitis, there’s an expanded section at the end of the diet tips. Also worth noting, as the title suggests, most of this advice applies to IBD, IBS, etc.
Ulcerative Colitis Diets: What to Eat?
No single “ulcerative colitis diet” will work for everyone. What’s important, is to find or discover through trial and error, the one that’s right for you. This is why it’s often difficult to know what to eat when you have a chronic illness like ulcerative colitis.
The good news is that there are several types of foods that are easy to digest and perhaps even help you feel better. All Ulcerative Colitis Diets should all start with the basics – with foods that help you maintain proper and adequate nutrition.
Every person’s overall health and well-being is dependent on nutrition. This is even more important when talking about an ulcerative colitis diet that minimizes or eliminates abdominal pain and other symptoms. These tips should not be used for anything other than educational purposes. To develop a safe, personalized meal plan, you MUST work with your doctor or a dietitian.
Food Journaling, Meal Planning & Food Preparation
Because each person’s symptoms and experience tend to be so different, your ability to find a successful ulcerative colitis diet plan depends on being organized and tracking your results. You need to have a plan, stick to that plan, document changes in symptoms and then change the plan accordingly. It will take commitment and experimentation.
- Keep A Food Journal – Track your food and symptoms in a journal. It doesn’t matter how you do this, as long as you do this. If you do nothing else, do this – keep the journal. Patterns will emerge. You will start to see which foods trigger symptoms or otherwise make them worse.
- Stay Hydrated – Water is life. So many health problems can be cured or minimized by simply drinking enough water. For those that don’t like water, you can also drink herbal teas (make sure to journal it) and tomato juice. Just make sure you’re getting plenty of fluid. Also, you should avoid straw and drink slowly so as not to swallow air.
- Eat Smaller Portions, More Often – Most people, regardless of their health, will feel better eating four to six small meals a day, for those ulcerative colitis this is even more true. Plus, it makes uncovering trigger foods even easier.
- Stay Stocked – Plan your shopping so you can keep your kitchen stocked with healthy foods that you enjoy. Since we tend to make our worst food choices when we’re hungry, staying stocked with only healthy food makes it effortless to choose right.
- Cook Simply – Don’t make it complicated. For your day to day needs, stick to healthy cooking techniques such as boiling, grilling, steaming, and poaching. Prepare meals in advance by cooking in large batches, or at least prep washing/cutting/cooking.
What To Eat During An Ulcerative Colitis Flare Up
While we often can’t control all the environmental factors in our lives, we certainly can control what we eat. By keeping your food journal, you will quickly learn that there are certain foods you should avoid during (or to prevent) a flare up. If you notice that eating that cheese pizza you love so much results in belly pain or abdominal cramps, you’ll most likely learn to stop eating cheese pizza. You will also learn that some foods will help you get the right amount of nutrients, vitamins, and minerals without making the symptoms worse.
You may want to consider eliminating certain foods from your diet as part of a dietary intervention (also known as an “elimination diet”). However, this type of dietary intervention should be part of a much broader treatment plan and you should only do this under the supervision of a healthcare professional or healthcare team that includes an experienced dietitian/nutritionist to ensure healthy nutrition and safety.
Most people will ultimately discover that for them, some specific foods trigger cramping, bloating, and/or diarrhea. Likewise, they will also realize that certain foods are easier to digest and provide the necessary nutrients the body needs.
All humans will benefit from eating a balanced diet. Additionally, most humans and especially those dealing with a dis-ease of inflammation like ulcerative colitis, will feel better following an anti-inflammatory diet.
5 Types of Foods You May Need to Avoid or Eliminate During a Flare Up
Again, there is no single diet to follow because every body is different, so this list doesn’t apply to every person all the time. You may find that you tolerate one common trigger food well, and another one brings intense abdominal symptoms. Listen to your body. Pay attention to changes in your bowel habits. Write it in your journal.
However, do take notice as you read this, just how much of this list is common sense health and nutrition we should all follow whether we have ulcerative colitis symptoms or not. While there are some restrictions, this not a particularly special diet therapy we’re talking about here. It’s only a special diet in so far as it works for you and helps you feel better.
- Avoid or Eliminate Alcohol & Caffeine – Society as a whole would be healthier if we avoided, minimized or eliminated beer, wine, liquor, caffeinated sodas, carbonated drinks with caffeine and coffee – but this is especially true for many with ulcerative colitis.
- Avoid or Eliminate Spicy Food – Some of our favorite foods are spicy. There’s nothing like some good, authentic Mexican salsa or your favorite Kung Pao Chicken. Or maybe you love hot sauces like Tabasco with your eggs in the morning, or Sriracha sauce on your sushi. While spicy foods have health benefits for many, others may need to avoid them.
- Avoid or Eliminate High-Fat, High-Sugar & Fried Foods – There’s no denying that fat and sugar taste good! But you definitely want to record all the butter, coconut, cream, dairy, pastries, candy and juice that you consume as they tend to trigger symptoms. Also, lactose in milk products can be especially troublesome, and fried foods too – we should all avoid or minimize fried food.
- Avoid or Eliminate Insoluble Dietary Fiber – This one is hard for most people because it’s counter to so much of what we “know” about eating healthy. Eat lots of fruits and raw vegetables! Right? Not in this case. Ulcerative colitis symptoms are often triggered by these foods because they are hard for the body to digest.- Raw fruits and veggies with a peel
– Dried fruits
– Fruits with skin and seeds
– Berries and cherries
– Raw green vegetables (especially cruciferous veggies like broccoli and cauliflower)
– Whole nuts
– Whole grainsAgain, keep your food journal, your experience may be different. - Avoid or Eliminate Non-absorbable Dietary Sugars: Non-absorbable sugars are also called sugar alcohols. While they taste sweet like normal sugar, unlike normal sugar these manufactured sugars are not readily absorbed from the intestines and digestive tract into the body. Most non-absorbable sugars are manufactured for commercial use and have names like sorbitol and mannitol. It’s also naturally present in some varieties of fruits and juices. In general you want to avoid or eliminate all manufactured and refined sugar. Watch out for:- Peaches, pears and prunes
– Sugar-free gum
– Ice cream
– Candy
– Processed fruit products
– Fruit drinks and soft drinks
5 Types of Foods You May Tolerate in Your Diet During a Flare Up
This list of diet recommendations may or may not work well for you. So, once again, keep your food journal and find out what works for you. When you go back and study your food journal, the patterns and results should become clear – this is how ulcerative colitis diets must be tailored to each person.
- Fruits with Low Fiber – You may find that you are able to enjoy fruit juices without pulp, canned fruit, cantaloupe, honeydew melon, watermelon, nectarines, papayas, peaches and cooked fruit.
- Lean Proteins – We all need to maintain a healthy protein intake. For those on a plant-based diet or even semi-vegetarian diet, you should do well with soy and firm tofu as solid sources of protein. If you want animal protein, then focus on fish, lean cuts of pork, white meat poultry and eggs.
- Refined Grains – Some people can eat various gluten-free breads and even sourdough or potato bread. Incredibly some can even consume white pasta, white rice, and oatmeal without issue, while others find that a gluten-free diet plan does wonders.
- Fully Cooked Vegetables – Here we want to look for seedless, skinless, non-cruciferous vegetables like carrots, spinach, onions, beets, potatoes, sweet potatoes, pumpkin, squash, celery, and chard.
- Nutritional Supplements – Ask your dietician or healthcare providers about what supplements may fit your needs towards preventing poor nutrition. Omega-3 fatty acids and turmeric are both great supplements for reducing inflammation.
Eating in Periods of Remission
If you’re in remission and your symptoms are light or even gone, give yourself the best chance at maintain that state by continuing to eat a nutritious and diverse diet. Consider the food you eat as the most powerful of medicines!
With all ulcerative colitis diets, we need to be sure work new foods in very slowly. Stay hydrated. Talk to your nutritionist, dietitian or healthcare professional before making any drastic changes to your diet, and of course, remember to keep up with your food journal.
These are examples of foods that may help you stay healthy, hydrated and in remission:
- Fruits & Vegetables – Try to eat the rainbow by consuming as many “colors” as possible. Peel everything.
- Foods High in Calcium – Eat dark green, leafy vegetables like cooked kale, spinach, and collard greens. If you can handle dairy products then yogurt, kefir, and milk can be good options as well.
- Lean Proteins – Again protein is very important. Soy and firm tofu are go-to options without meat. Otherwise fish, lean cuts of pork, white meat poultry and eggs are all great options.
- Probiotics – Some foods naturally contain probiotics, or commonly have probiotics added to them, including yogurt, kefir, kombucha, sauerkraut, pickles, miso, tempeh, sourdough bread and some cheeses.
- Foods High in Soluble Fiber – Unless you’ve been advised otherwise, you may be able to enjoy whole grains, nuts, oat bran, beans, barley peas, beans, apples, citrus fruits, carrots, barley and psyllium.
- Olive Oil – There has been plenty of rigorous study on how linoleic acid in olive oil (also walnuts, egg yolks, and coconut oil) often lowers inflammatory markers and helps with UC symptoms. “Good” fat is essential but don’t go crazy because too much can cause inflammation.
—–
The following section is intended to provide information and context for those who may be a bit unfamiliar with ulcerative colitis or perhaps just to help confirm and round out your knowledge. There’s also some useful background information about diagnosis, medication, living with ulcerative colitis. As a holistic healer, I am not anti or against Western medicine, but rather, I seek to work in compliment with it as one of the many tools available to cure dis-ease.
Ulcerative Colitis, Crohn’s Disease or Something Else?
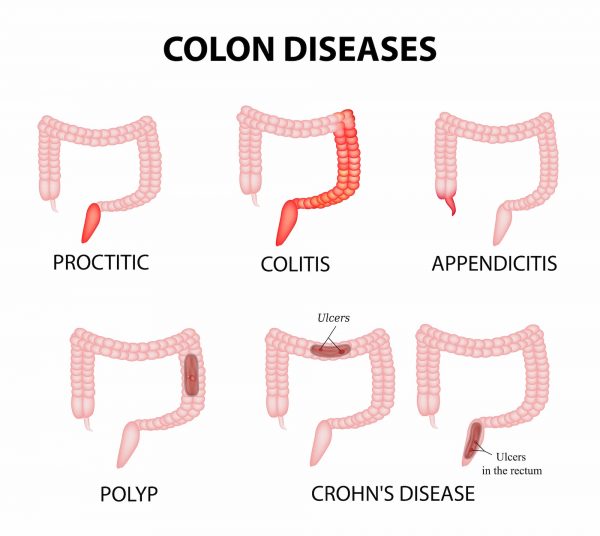
The colon, also known as the large intestine, has three parts or section: ascending colon (left side), transverse (horizontal), descending colon (right side), and the sigmoid colon (horizontal) just before the rectum.
Ulcerative colitis symptoms in each person will be different depending on where inflammation occurs and how bad it is. The most common symptoms include:
- Diarrhea, often persistent and with blood or pus
- Abdominal pain and cramps
- Rectal pain and/or rectal bleeding
- More frequent bowel movements
- Urgency to defecate
- Inability to defecate despite urgency
- Weight Loss
There are common complications that tend to come with UC, even though they are not actually a direct result of this chronic health condition. Fever, fatigue, and anemia are perhaps the most common additional symptoms. Additionally, inflammation beyond the colon often shows up as skin sores, skin rashes, mouth sores, joint pain, red and painful eyes, and sometimes even liver disease.
While both are referred to as inflammatory bowel disease or IBD, and Ulcerative colitis is related to Crohn’s disease, they are still different. Crohn’s disease, unlike ulcerative colitis, is not limited to the colon and is a chronic inflammatory disease of the intestines or the entire GI tract. Crohn’s often affects the small intestine and colon although occasionally it, too, is limited to the colon.
You may have also heard of irritable bowel syndrome or IBS, which also presents with abdominal pain and diarrhea as its main symptoms. But, irritable bowel syndrome is currently considered a malfunction of the nerves and muscles of the intestines because there’s no inflammation.
Who Gets Ulcerative Colitis And Why?
UC like all other health conditions is caused by various underlying factors including unresolved infections, toxins, nutritional deficiencies and emotional patterns.
Ulcerative colitis is an inflammatory bowel disease (IBD) that occurs mostly in developed nations, and is more common in urban centers where the Western diet pattern dominates. It is estimated that approximately 1 million people in the U.S. alone suffering from the disease and its many gastrointestinal symptoms.
As a chronic illness, UC can be active at times and inactive at other times. If the symptoms are mild, they do not make the body “burn out.” The unpredictable nature of ulcerative colitis makes diagnosis very challenging.
The disease may start at any age, but individuals with the disease usually develop it between 15 and 25.
It seems that there is a genetic component to ulcerative colitis because individuals of eastern European Jewish lineage have a great risk of ulcerative colitis. While the cause is still unknown, research has hinted at a connection to irregular reactions to bacteria in the colon. Evidence does not indicate that one’s diet is the cause of ulcerative colitis.
To diagnose ulcerative colitis a colonoscopy is usually ordered, during which an endoscope (a long flexible tube) is passed through the anus and into the colon. While ulcerative colitis can be diagnosed by X-rays of a barium-filled colon, colonoscopy should be used because they are more sensitive and allow for biopsies to be taken of the lining of the colon.
During a flare of the disease it’s important to get treatment in order to avoid serious complications. A lot of the time, bleeding is the most common problem. which can often lead to anemia. During an extreme flare up, the colon can get so swollen it stops working altogether. The longer it is left untreated, the more likely the blockage will become a medical emergency or require surgery. If not treated, the problem could become severe or even life-threatening.
Ulcerative colitis is also one of the major risk factors of colon cancer; as the disease progresses, the risk grows. Regular annual screening is recommended for those who are at high risk of developing the disease, usually starting eight years after the onset of UC, maybe sooner depending on age.
Inflammation problems in other parts of the body not directly connected with the colon often occur as a consequence of ulcerative colitis. Specifically, the spine and large joints can be compromised by this inflammation, and some will even experience major skin ulcerations.
Ulcerative Colitis Medications & Surgery
The goal of all ulcerative colitis treatment is to reduce colonic inflammation. The most effective drugs or medicines for this purpose are the salicylates, which are related to aspirin.
When aminosalicylates do not work, corticosteroids are used. A third type of anti-inflammatory drug known as immunomodulators are also used, but it may take weeks or months for these drugs to work.
The latest technology in the treatment of ulcerative colitis is the use of biologic drugs, which target the body’s immune system in order to help heal ulcerative colitis.
Biologic therapy must be given intravenously every few weeks, and involves administering antibodies that are directed at the molecules produced by the immune system that cause inflammation.
Inspired by low incidence of UC in developing countries, there are ongoing clinical studies into the possibility that the pig whipworm may be useful as ulcerative colitis treatment because some scientists theorize that worms in the colon change the immune response and consequently reduce inflammation in the process. 42% of UC patients in one study saw their symptoms improve after eating pig whipworm eggs for three months.
Unfortunately, even with all the treatments available, 1 out of 3 people with UC will ultimately need surgery to address the inflammation, to prevent or treat cancer, or because of complications like a ruptured colon or bowel obstruction. The colon is often removed, which one could say “cures” a person of ulcerative colitis. Fortunately, the colon can now be removed with no need for an ileostomy; it used to be that people were left with a lifetime of ileostomies, which are external bags that the small intestine emptied into.
Ulcerative Colitis in Children
Without proper care, pediatric ulcerative colitis will result in slower than normal growth and/or stunted growth. Intestinal inflammation lowers a child’s appetite, which mean less food is eaten resulting in fewer nutrients to support healthy growth. Supplements are often a good idea as is making sure that enough calories are consumed, which sometimes requires a high-calorie diet for some kids. Additionally, a therapy or counseling may be sought to help a child develop the tools to cope with their disease.
Practical Considerations for Treating & Controlling Ulcerative Colitis
The fact is that there are precious few drug-free tools that can reduce symptoms and improve the inflammatory condition characterized by this disease. Yes, diet and nutrition are critical – you should think of them as a combination of medication – they are equally important.
Stress is another huge factor. It is important to reduce stress in order to make the symptoms less severe. It is of paramount importance for patients to their treatments regularly and not deviate. Also, while smoking has been shown to reduce some of the inflammation of ulcerative colitis, for obvious health reasons it’s definitely not a recommended treatment.
There is a link between diet and the day to day health condition of someone living with ulcerative colitis. Once again, a food diary is essential so you can document when certain foods make your symptoms worse – eliminate them! Without a food diary this is difficult to do as we don’t always have good food memory.
It’s possible that people with UC who are sensitive to the sugar in milk, such as Lactose, may be experiencing symptoms similar to those of ulcerative colitis. Despite not being the cause of the ulcerative colitis, eliminating milk may help some people.
It’s important to make sure the diet you follow is good for you, and it may require the professional help of a nutritionist or dietician experienced with needs of UC patients.
Iron deficiency may be caused by the loss of red blood cells in the colon due to the bleeding caused by ulcerative colitis so it may be necessary to add more iron to your diet. Supplements of vitamins and minerals may be necessary and useful, because many of drugs used to treat ulcerative colitis can reduce the absorption of nutrients in general.
Probiotics
Probiotics consist of bacteria that confer a health benefit on the person who ingests them. They’re usually found in the human intestine. Probiotics have proven medical benefits when used to treat a variety of medical conditions. People with ulcerative colitis are often able to maintain their remissions with the help of probiotics in their gut flora. While probiotics are found in yogurts and some other foods, the probiotics that have been shown to be the most medically beneficial are sold separately as supplements and are not food products. The exact bacteria that are present have a huge impact on the effects of probiotics. Many probiotics that are sold have no beneficial effect, and therefore the one that is used for treatment needs to be chosen carefully.
Hydration
Hydration is a critical factor in all human health. With UC, chronic persistent diarrhea often causes dehydration, especially when feeling ill and not eating or drinking enough liquids. Maintaining an adequate fluid intake is crucial. Both the amount and color of urine can be used as a guide as to whether or not there’s enough fluid intake. If the urine is dark or low in volume, more liquids are needed. As a general rule, half an ounce per pound of weight should be drank daily, and even more when diarrhea is an active disease symptom. Consider water and hydration as important as your medication.
Living With Ulcerative Colitis
Ulcerative colitis often has a negative impact on your relationships, especially an intimate relationship. Feeling generally or needing to go to the bathroom frequently can be limiting but managed through appropriate treatment. Additionally, it’s important to note that some medications, like corticosteroids for example, can affect your mood resulting in depression or euphoria. Reduced libido is also possible. All this to say, it’s a good idea to try to be as open and direct as possible about these issues with your intimate partner, doctors and those closest to you. It might even be a good idea to consider seeing a psychologist or psychiatrist to help you cope if you are struggling.
Traveling With Ulcerative Colitis
When in remission, people with ulcerative colitis usually have no problems with travel. Several precautionary steps may be necessary if some symptoms are present.
- Plan & Prepare – Before arriving at airports and other public buildings, find out ahead of time using the internet, or by asking employees and others where the bathrooms and other resources you need are located. This way if one of those urgent bowel movements arises you’ll know ahead of time exactly where to go.
- Wet Wipes – Make sure to keep a change or two of underwear and wet wipes (moist towelettes) in your carry-on.
- Medication – Be sure to bring enough medication for the entire trip and bring copies of prescriptions in case of an emergency to streamline your access.
- Ask For Tips – Ask your healthcare team (nutritionist, dietician, doctor) if they have any specific tips or recommendations for you.